What is Subcutaneous Insulin Injection?
Subcutaneous insulin injection is a method of delivering insulin medication into the subcutaneous fat layer using specialized insulin injection devices. This approach represents the gold standard for insulin therapy among diabetes patients worldwide. According to the World Health Organization, approximately 463 million people globally have diabetes, with roughly 30% requiring insulin-dependent treatment.
The subcutaneous route has become the preferred method because the subcutaneous fat layer contains a rich vascular network that allows for stable insulin absorption into systemic circulation. This method avoids the complexity of intravenous administration while preventing the potential pain associated with intramuscular injections. When performed correctly, subcutaneous insulin delivery begins working within 30-60 minutes, providing consistent blood glucose control.
Selecting the Right Insulin Injection Device
1. Insulin Pens vs Traditional Insulin Syringes
Insulin Pen Systems
- Advantages: User-friendly operation, portable design, precise dosing accuracy
- Target Population: Beginners, visually impaired patients, frequent travelers
- Market Penetration: Over 85% adoption rate in developed countries for insulin delivery devices
Traditional Insulin Syringes
- Advantages: Cost-effective, compatible with insulin mixing protocols
- Disadvantages: Complex operation, higher error rates
- Target Population: Budget-conscious patients, those requiring mixed insulin therapy
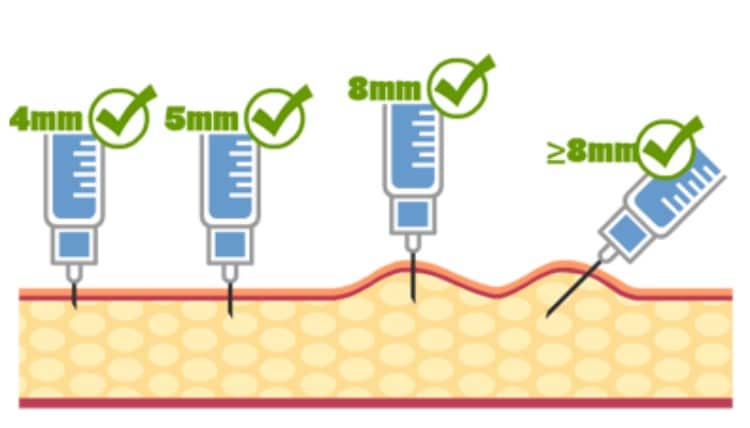
2. Needle Selection for Subcutaneous Injection
Needle specifications directly impact injection efficacy and patient comfort:
Needle Length Parameters
- 4mm: Optimal for pediatric patients and lean adults
- 5-6mm: Standard recommendation for most adult patients
- 8mm+: Suitable for obese patients, requires skin pinching technique
Needle Gauge Specifications
- 31G-32G (0.23-0.25mm): Ultra-fine, minimal pain sensation
- 30G (0.3mm): Balanced comfort and flow rate
- 29G (0.33mm): Appropriate for high-viscosity insulin formulations
Four Critical Issues in Subcutaneous Insulin Administration
Issue #1: Improper Injection Site Selection and Rotation
Problem Prevalence Clinical studies indicate that approximately 60% of diabetes patients demonstrate inadequate injection site rotation practices, resulting in subcutaneous nodules and lipodystrophy.
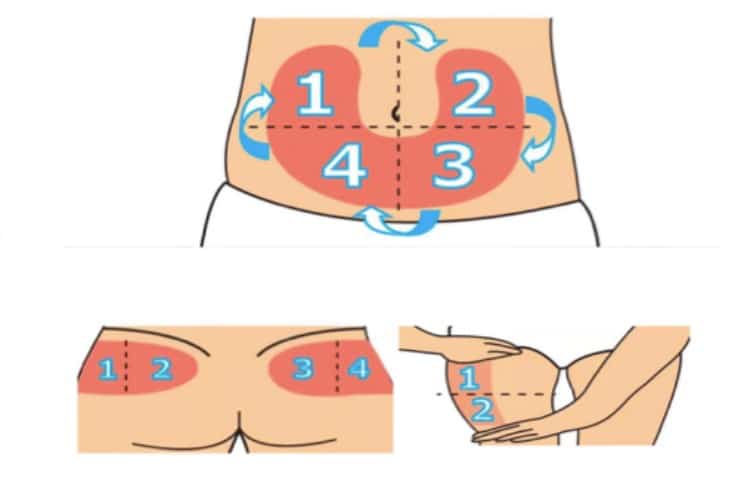
Optimal Injection Sites
- Abdomen: 5cm radius around navel, fastest and most consistent absorption
- Lateral Thigh: Moderate absorption rate, ideal for long-acting insulin
- Upper Arm (Lateral): Requires assistance, rapid absorption characteristics
- Buttocks: Slowest absorption, suitable for basal insulin therapy
Rotation Protocol
- Maintain minimum 1cm spacing between injection sites
- Follow systematic rotation patterns, avoid random selection
- Absorption variability between sites can range 20-30%
Issue #2: Injection Depth Control Errors
Problem Identification Research demonstrates that approximately 25% of patients experience injection depth inconsistencies, leading to unpredictable insulin absorption patterns.
Depth Control Parameters
- Subcutaneous Layer Thickness: Normal adult range 5-15mm
- Injection Angle: Perpendicular (90°) administration is standard protocol
- Skin Pinching Technique: 4-5mm needles typically don’t require pinching; 6mm+ needles recommend skin elevation
Consequences of Improper Depth
- Intramuscular injection (too deep): 50-100% faster absorption, hypoglycemia risk
- Intradermal injection (too shallow): Incomplete absorption, poor glycemic control
- Muscle injection demonstrates significantly accelerated absorption compared to subcutaneous delivery
Issue #3: Inaccurate Injection Timing
Problem Assessment Clinical surveys reveal that over 40% of patients misunderstand insulin timing requirements, compromising blood glucose management outcomes.
Insulin-Specific Timing Protocols
- Rapid-Acting Insulin: 5-10 minutes pre-meal, 15-minute onset
- Short-Acting Insulin: 20-30 minutes pre-meal, 30-minute onset
- Intermediate-Acting Insulin: 1-2 hour onset, 12-16 hour duration
- Long-Acting Insulin: 1-2 hour onset, 18-24 hour duration
Timing Precision Impact
- 10-minute timing deviations can cause 1-2 mmol/L postprandial glucose fluctuations
- Irregular injection schedules increase glycemic variability by 15-25%

Issue #4: Dosage Adjustment and Blood Glucose Monitoring Disconnect
Problem Documentation Approximately 35% of patients demonstrate inadequate insulin dose adjustment practices, primarily failing to modify doses based on glucose patterns.
Evidence-Based Adjustment Principles
- Basal Dose Titration: Adjust long-acting insulin based on fasting glucose
- Prandial Dose Modification: Adjust meal-time insulin for postprandial control
- Correction Doses: Implement temporary adjustments for current glucose levels
Monitoring Frequency Guidelines
- Unstable Control Period: 4-7 daily measurements
- Stable Control Period: 2-3 weekly measurements
- HbA1c Target: <7% (may be relaxed to <8% for specific populations)
Common Dosage Errors
- Dose adjustment hesitancy: 45% of patients never self-adjust
- Excessive adjustment increments: Recommend 10-20% maximum changes
- Inadequate glucose logging: Complete records improve control by 30%

Key Takeaways for Optimal Subcutaneous Insulin Therapy
Subcutaneous insulin injection appears straightforward but encompasses sophisticated scientific principles and technical requirements that directly influence glycemic control effectiveness. Mastering these four critical areas—injection site rotation, depth control, timing precision, and dose adjustment—can significantly enhance insulin therapy outcomes.
Recommendations for Healthcare Providers and Patients:
- Implement regular insulin injection technique training programs
- Establish comprehensive blood glucose monitoring systems
- Maintain consistent communication with healthcare teams
- Customize treatment protocols based on individual patient needs
Only through proper subcutaneous insulin administration techniques can patients achieve optimal therapeutic outcomes and improved quality of life in diabetes management.






